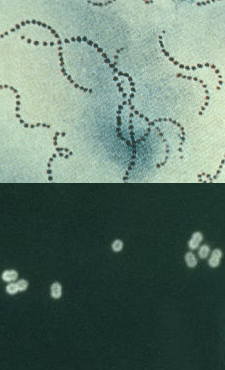
 Top: Streptococcus pyogenes
Top: Streptococcus pyogenesCDC ID#2109
Bottom: Streptococcus pneumoniae
CDC ID#3149, Dr. M. S. Mitchell
- Streptococci are Gram-positive, non-motile cocci that divide in one plane, producing chains of cells. S. pneumoniae is a lancet-shaped diplococcus (formerly genus Diplococcus).
- The streptococci are catalase negative (unlike Staphylococcus) and may be either facultative or obligate anaerobes.
- Hemolysis (alpha, beta) on blood agar is an important differential characteristic.
- Lancefield groupings are based on the serology of cell wall polysaccharides (18 groups were originally established by Rebecca Lancefield).
- The M proteins of group A serve as important virulence factors that help the organism resist phagocytosis.
- Lipoteichoic acids (LTA) mediate attachment to epithelial cells.
- Many antigenic moieties on the streptococcal cell surface resemble human muscle and connective tissue and these similarities may be responsible for the late sequelae. For example, S. pyogenes membrane Ags resemble cardiac, skeletal, smooth muscle, heart valve fibroblasts and neuronal tissue.
- The capsule of S. pyogenes is composed of hyaluronic acid (like host connective tissue) so it is non-antigenic while the capsule of S. pneumoniae is very antigenic and is its sole virulence factor.
- Toxins produced by streptococci include: streptolysins (S & O), NADase, hyaluronidase, streptokinase, DNAses, erythrogenic toxin (causes scarlet fever rash by producing damage to blood vessels; requires cell to be lysogenized by phage that encodes toxin).