Introduction to Medical Microbiology
A BIT OF HISTORY
| 1680s: |
Leeuwenhoek discovers bacteria. |
|
| 1720s: |
Benjamin Martin describes a germ theory of disease in his book A New Theory of
Consumptions: More Especially of a Phthisis or Consumption of the Lungs: |
|
|
"The Original or Essential Cause, then, which some content themselves to call a serious
disposition of the Juices, others a Salt Acrimony, others a strange Ferment, others a Malignant
Humour, may possibly be some certain Species of Animalculae or wonderful minute living
creatures that, by their peculiar Shape or disagreeable Parts are inimicable to our Nature; but,
however, capable of subsisting in our Juices and Vessels"
"The minute Animals or their Seed . . . are for the most part either conveyed from Parents to
their Offspring hereditarily or communicated immediately from Distempered Persons to sound
ones who are very conversant with them. . .It may, therefore, be very likely that by an habitual
lying in the same Bed with a consumptive Patient, constantly eating or drinking with him or by
very frequent conversing so nearly as to draw in part of the Breath he emits from the Lungs, a
Consumption may be caught by a sound person." |
|
| 1860‑1885: |
Louis Pasteur "invents" pasteurization and develops vaccines for rabies and anthrax, supporting the germ theory |
|
| 1890s: |
Robert Koch sets guidelines for how to prove that a particular microbial agent is
responsible for a particular disease. Koch's postulates state that:
- The suspect microorganism must be routinely isolated from patients with a particular illness;
- The microorganism must be grown in pure culture in vitro;
- When the pure culture is inoculated into a new host, it must cause the same illness;
- The same microorganisms must be reisolated from new host.
|
|
| 1929: |
Alexander Fleming discovers penicillin. |
|
| 1939: |
Florey and co-workers find a way to isolate penicillin. |
|
HOST-PARASITE RELATIONSHIPS
| |
MICROBES |
| Triangle of relationships |
 |
|
 |
| |
HUMANS |
 |
DRUGS |
MECHANISMS OF PATHOGENESIS
Pathogenic properties of bacteria: microorganisms cause disease by two basic mechanisms: 1)
invasion of tissue and 2) production of toxins.
Invasiveness: the ability to invade host tissues.
- Intracellular pathogens vs extracellular pathogens: Intracellular pathogens generally produce
chronic disease, extracellular pathogens generally produce acute disease (e.g. Mycobacterium tuberculosis vs
Streptococcus pyogenes).
- Capsules: Some bacteria produce hydrophilic gels that inhibit phagocytosis (e.g. smooth vs
rough strains of Streptococcus pneumoniae).
- Adaptation: microenvironments of the host body provide habitats for bacteria that are capable
of selective tissue invasion (e.g. Neisseria meningitidis vs Streptococcus pneumoniae. Both
inhabit the human nasopharynx, but only the latter invades the lower respiratory tract).
- Extracellular enzymes: Some bacteria produce enzymes like hyaluronidase or collagenase that
degrade host tissues.
Toxigenicity: the production of toxins.
- Exotoxins: secreted proteins that are generally very toxic but heat labile. they are usually very good immunogens. Exotoxins are found mostly in Gram-positive organisms.
- Endotoxins: complex polysaccharides (LPS) that are a part of the bacterial cell wall. they are usually poorly immunogenic. These toxins are released when cells lyse, are generally heat stable, and found mostly in Gram-negative bacteria.
Virulence: the combination of invasiveness and toxigenicity producing the ability to overcome
host defenses.
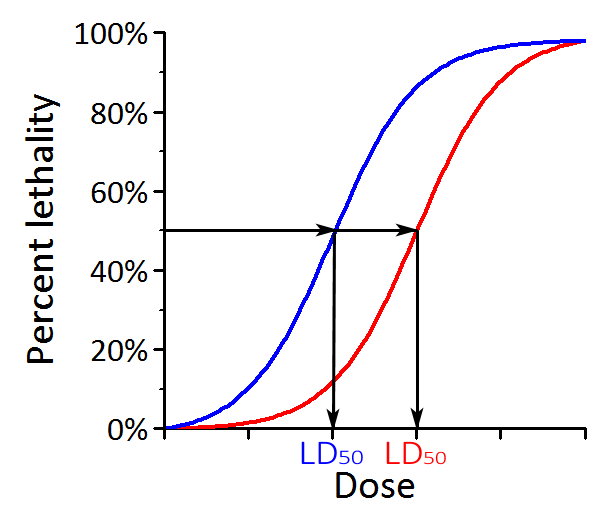
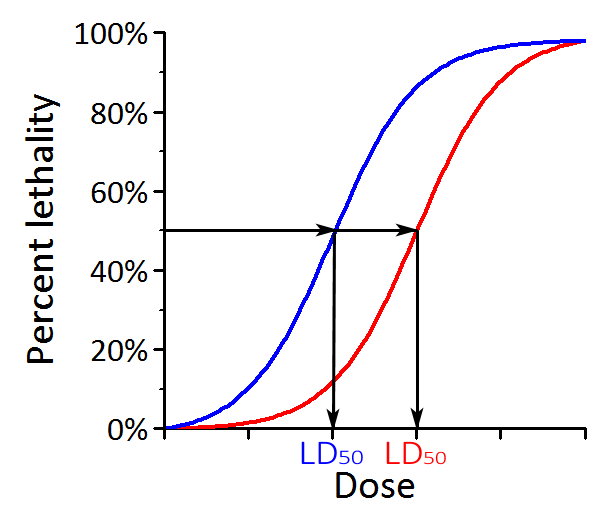
- Measurement of virulence: LD50 (% dead vs dose).
- Variability in virulence potential may be genotypic (e.g. smooth vs rough strains of
Streptococcus pneumoniae, lysogeny in Corynebacterium diphtheriae) or phenotypic (e.g. the
production of capsular polysaccharides in the presence of rich carbohydrates).
HOST DEFENSES
Host defenses include both physiologic barriers and immunological responses. Some defenses
are non-specific, others are highly specific. Host defenses can vary considerably due to many factors
including alcohol, drugs, nutrition, immunologic disorders, etc.
Skin and mucous membranes provide the first line of defense through:
- Mechanical factors: physical barrier to penetration.
- Chemical factors: gastric acidity, unsaturated fatty acids, lysozyme.
- Microbial factors: antagonism by normal flora.
Phagocytic cells provide a secondary line of defense by consuming invaders and secreting
substance that produce immune responses:
- Mononuclear cells: monocytes (blood) and macrophages (tissue).
- Neutrophils: polymorphonuclear (PMN) granulocytes.
- Inflammation: immune response producing dilation of blood vessels, increased vascular
permeability and diapedesis of monocytes.
- Phagocytosis: cells destroy invaders by i) utilizing specific membrane receptors for
attachment (e.g. immunoglobulin Fc and complement C3b receptors) and ii) ingesting invaders
into phagocytic vacuoles, leading to intracellular killing by fusion with lysosome-like granules
containing lowered pH, peroxide, enzymes, etc.
Humoral factors: antibody mediated defenses include:
- Antitoxins: specific antibodies that bind certain exotoxins.
- Bacteriolytic antibodies: antibodies plus complement can directly lyse Gram-negative cells.
- Opsonizing antibodies: coat cell surface and enhance phagocytosis (Fc receptors).
Cell-mediated factors: cell-mediated defenses include:
- Cytotoxic T-lymphocytes: specific cells capable of destroying altered host cells.
- K and NK cells: lyse altered or transplanted host cells.
- Activated macrophages: phagocytes that possess a greatly enhanced capacity for intracellular
destruction of ingested microorganisms.
TRANSMISSION OF DISEASE
Communicability: infectious disease can be transmitted either directly (e.g. person to person) or indirectly (e.g. contaminated water). Factors involved in the communicability of an infectious agent include:
- Source, including dormant or latent infections (carriers).
- Number of infectious agents released from a host.
- Capability of surviving transit from host to host.
- Percentage of the host population that is susceptible to the agent.